What Is Involved In A Total Pelvic Exenteration (TPE)
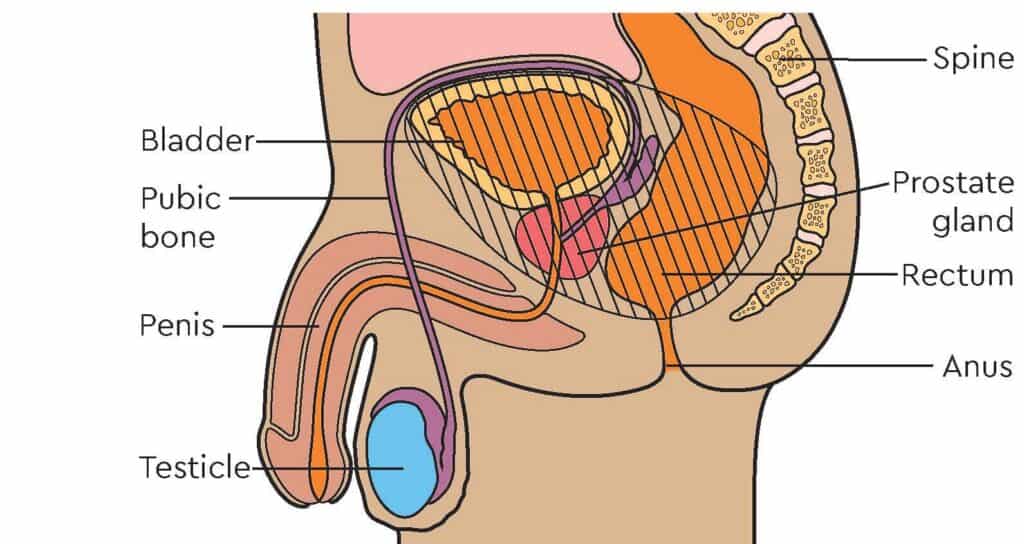
A total pelvic exenteration (TPE) is an extensive surgical procedure performed to treat advanced or recurrent pelvic malignancies that have not responded to other treatment options. It involves the removal of multiple organs within the pelvic cavity, including the rectum, anus, bladder, and reproductive organs (uterus, cervix, ovaries, and part of the vagina in women, and prostate in men).
Additionally, nearby lymph nodes and surrounding tissues may also be excised to ensure all cancerous cells are removed. The decision to perform a total pelvic exenteration is not taken lightly, as it is a complex and highly invasive procedure with significant risks and potential complications. It is typically reserved for cases in which the cancer has extensively invaded the pelvic organs and adjacent structures, and when there are no other feasible treatment options available.
The decision to perform a total pelvic exenteration is not taken lightly, as it is a complex and highly invasive procedure with significant risks and potential complications. It is typically reserved for cases in which the cancer has extensively invaded the pelvic organs and adjacent structures, and when there are no other feasible treatment options available.
Total Pelvic Exenteration: Surgical Process
A Total Pelvic Exenteration is complex and extensive operation. It takes several hours and several surgeons with specialised knowledge and skills.
The surgery is performed under general anesthesia and involves several stages:
Preoperative Evaluation: Before undergoing a total pelvic exenteration, the patient undergoes a thorough preoperative evaluation, which may include physical examinations, imaging tests (such as CT scans, MRI, or PET scans), and biopsy to confirm the extent and stage of the cancer.
Preparation: The patient is prepped for surgery, which involves cleansing the surgical site and administering antibiotics to prevent infection.
Incision: The surgeon makes an incision in the abdominal wall to gain access to the pelvic cavity.
Organ Removal: The surgeon carefully removes the affected organs and tissues within the pelvic cavity, such as the bladder, rectum, reproductive organs, and nearby lymph nodes. In some cases, a portion of the pelvic bone may also be removed to ensure complete resection.
Reconstructive Surgery: After removing the diseased organs, the surgeon performs reconstructive surgery to restore some bodily functions and improve the patient’s quality of life. Several reconstructive techniques can be employed, such as:
Urinary diversion: Creating a new way for urine to exit the body. Common methods include creating an ileal conduit (using a segment of the small intestine as a passage for urine to be collected in an external pouch) or a neobladder (creating a reservoir from a segment of intestine to act as a new bladder).
Colostomy or ileostomy: If the rectum and colon are removed, a stoma is created on the abdominal wall to divert waste into a colostomy or ileostomy bag.
Vaginal reconstruction: For women, reconstructing the vagina using tissues from other parts of the body may be performed to maintain sexual function and improve quality of life.
Closure: After completing the surgical procedures, the incisions are closed with sutures or staples.
Recovery from a total pelvic exenteration is challenging and typically involves a prolonged hospital stay. Patients may require extensive rehabilitation and support to adapt to the changes in their bodily functions. They might also need emotional and psychological counseling to cope with the significant impact on their quality of life.
As with any major surgery, there are risks involved with a total pelvic exenteration, including infection, bleeding, blood clots, damage to nearby organs or nerves, and postoperative complications like bowel obstruction or urinary leakage. The procedure is physically demanding and can lead to significant changes in urinary, bowel, and sexual functions, depending on the extent of reconstruction.
Due to the complexity and potential complications of a total pelvic exenteration, patients and their medical teams must carefully weigh the potential benefits against the risks before deciding to proceed with the surgery. Patient selection is critical, and candidates should be in good overall health to tolerate the procedure and the subsequent recovery process.
The Use of Natural Therapies Post Total Pelvic Exenteration
Natural therapies can complement traditional medical care and support post-operative recovery from total pelvic exenteration in various ways. However, it’s essential to consult with your healthcare provider before incorporating any natural remedies, especially after a major surgery like a total pelvic exenteration. Here are some natural therapies that may aid in post-operative recovery:
Proper Nutrition: A balanced and nutrient-rich diet is crucial for healing and tissue repair. Focus on consuming a variety of fruits, vegetables, lean proteins, whole grains, and healthy fats. Adequate protein intake is especially important for wound healing. Consider consulting with a registered dietitian to create a personalised meal plan that meets your specific nutritional needs.
Chinese/Western Herbal Therapy: Some herbs have potential anti-inflammatory and healing properties. However, their use should be discussed with your healthcare provider to ensure they do not interfere with any medications or negatively impact your recovery. Turmeric, ginger, and bromelain are examples of herbs that may help reduce inflammation.
Probiotics: Antibiotic use during and after surgery can disrupt the gut microbiome. Probiotics can aid in restoring a healthy balance of gut bacteria, which may positively influence the immune system and reduce the risk of infection. Yogurt, kefir, or probiotic supplements are common sources of probiotics.
Aromatherapy: Certain essential oils, when used cautiously and under professional guidance, may help manage pain, reduce stress, and promote relaxation. Lavender and chamomile are popular choices for their calming effects.
Mind-Body Techniques/Meditation: Practices like meditation, deep breathing exercises, and guided imagery can help reduce stress and anxiety, which may support overall healing. They can also assist in managing pain and improving sleep quality.
Gentle Exercise: Depending on your surgical recovery guidelines, engaging in gentle exercises, such as walking or light stretching, can promote blood circulation, prevent complications like blood clots, and help maintain muscle tone.
Cold and Heat Therapy: Ice packs can reduce inflammation and ease pain when applied to the surgical site, while heat therapy (such as warm compresses) can help relax muscles and improve blood flow to promote healing.
Acupuncture: Acupuncture, when performed by a trained and licensed practitioner, may aid in pain management and support the body’s healing processes.
Hydration: Staying well-hydrated is essential for post-operative recovery, as it helps flush out toxins and promotes healing.
Social Support: Emotional support from family, friends, or support groups can have a positive impact on your mental well-being and overall recovery.
Research Into The Effectiveness of Herbs In The Treatment of Cancer
Take a look at the Journal Articles below – simply click on the title to view the Journal Article.
- Therapeutic Effects of Ten Commonly Used Chinese Herbs and Their Bioactive Compounds on Cancers.
- Medicinal Herbs Used in Traditional Management of Breast Cancer: Mechanisms of Action.
- Herb-sourced emodin inhibits angiogenesis of breast cancer by targeting VEGFA transcription.
- Anticancer Effects and Mechanisms of Berberine from Medicinal Herbs: An Update Review.
- The pharmacological mechanism of Chinese herbs effective in treating advanced ovarian cancer: Integrated meta-analysis and network pharmacology analysis.
- Berberine in combination with cisplatin induces necroptosis and apoptosis in ovarian cancer cells.
- Growth Inhibitory Efficacy of Chinese Herbs in a Cellular Model for Triple-Negative Breast Cancer.
- An in vivo molecular response analysis of colorectal cancer treated with Astragalus membranaceus extract.
- Chinese Herbs Interfering with Cancer Reprogramming Metabolism.
Potentially Useful Herbs Pre- and Post Total Pelvic Exenteration Surgery
Before and after a Total Pelvic Exenteration (TPE) surgery, certain herbs may be considered to support the patient’s well-being and enhance recovery. However, it’s crucial to consult with your healthcare provider before using any herbs, as they may interact with medications, affect blood clotting, or have other contraindications. Here are some herbs that are occasionally considered for pre and post-operative support:
Herbs used prior to Total Pelvic Exenteration surgery:
-
Arnica (Arnica montana): Arnica is sometimes used to reduce bruising and swelling associated with surgery. However, it should not be taken orally, as it can be toxic. Instead, topical arnica preparations are applied to the skin.
-
Ginseng (Panax ginseng): Ginseng may help improve physical endurance and reduce fatigue, which could be beneficial in preparing for surgery. However, it should be used cautiously, as it can affect blood pressure and interact with medications.
-
Turmeric (Curcuma longa): Turmeric contains curcumin, which has anti-inflammatory properties. It may help reduce inflammation and support the immune system. Turmeric supplements or teas are commonly used.
-
Ginger (Zingiber officinale): Ginger has anti-inflammatory and anti-nausea properties. It may help alleviate nausea and vomiting associated with anesthesia. Ginger tea or capsules can be considered.
-
Milk Thistle (Silybum marianum): Milk thistle is often used to support liver health. It may help the liver process medications and anesthesia more effectively.
Herbs used following Total Pelvic Exenteration surgery:
-
Arnica (Arnica montana): As mentioned earlier, topical arnica preparations may be used post-operatively to reduce bruising and swelling.
-
Calendula (Calendula officinalis): Calendula ointment can be applied topically to surgical wounds to promote healing and reduce infection risk.
-
Chamomile (Matricaria chamomilla): Chamomile tea or chamomile-based ointments may help soothe anxiety and promote relaxation, aiding in post-operative recovery.
-
Aloe Vera (Aloe barbadensis miller): Aloe vera gel can be applied topically to surgical wounds to soothe and promote healing.
-
Echinacea (Echinacea spp.): Echinacea is sometimes used to support the immune system post-operatively, although research on its effectiveness is mixed.
-
Peppermint (Mentha × piperita): Peppermint tea may help alleviate post-operative nausea and indigestion.
-
Lavender (Lavandula angustifolia): Lavender essential oil or lavender-infused products can be used to promote relaxation and reduce anxiety, potentially aiding in recovery.
-
Licorice (Glycyrrhiza glabra): Licorice root may have anti-inflammatory properties and can be used to soothe digestive discomfort post-operatively.
-
Witch Hazel (Hamamelis virginiana): Witch hazel can be applied topically to surgical wounds to reduce inflammation and soothe the skin.
Remember that herbal remedies should be used cautiously and under the guidance of a qualified herbalist or healthcare provider. Dosages, forms (tea, tincture, capsules, topical), and timing of herbal use should be tailored to your specific needs and discussed with your medical team.
Additionally, always disclose your use of herbs to your healthcare provider, as they can interact with medications and affect your overall health. While herbs may offer potential benefits, they should be seen as complementary to conventional medical care, especially in the context of major surgeries like Total Pelvic Exenteration.



